Future Pandemics Will Have The Same Human Causes As Ancient Outbreaks
Posted on Categories Discover Magazine
The last pandemic was bad, but COVID-19 is only one of many infectious diseases that emerged since the turn of this century.
Since 2000, the world has experienced 15 novel Ebola epidemics, the global spread of a 1918-like influenza strain and major outbreaks of three new and unusually deadly coronavirus infections: SARS, MERS and, of course, COVID-19. Every year, researchers discover two or three entirely new pathogens: the viruses, bacteria and microparasites that sicken and kill people.
While some of these discoveries reflect better detection methods, genetic studies confirm that most of these pathogens are indeed new to the human species. Even more troubling, these diseases are appearing at an increasing rate.
Despite the novelty of these particular infections, the primary factors that led to their emergence are quite ancient. Working in the field of anthropology, I have found that these are primarily human factors: the ways we feed ourselves, the ways we live together, and the ways we treat one another. In a forthcoming book, “Emerging Infections: Three Epidemiological Transitions from Prehistory to the Present,” my colleagues and I examine how these same elements have influenced disease dynamics for thousands of years. Twenty-first century technologies have served only to magnify ancient challenges.
Neolithic Infections
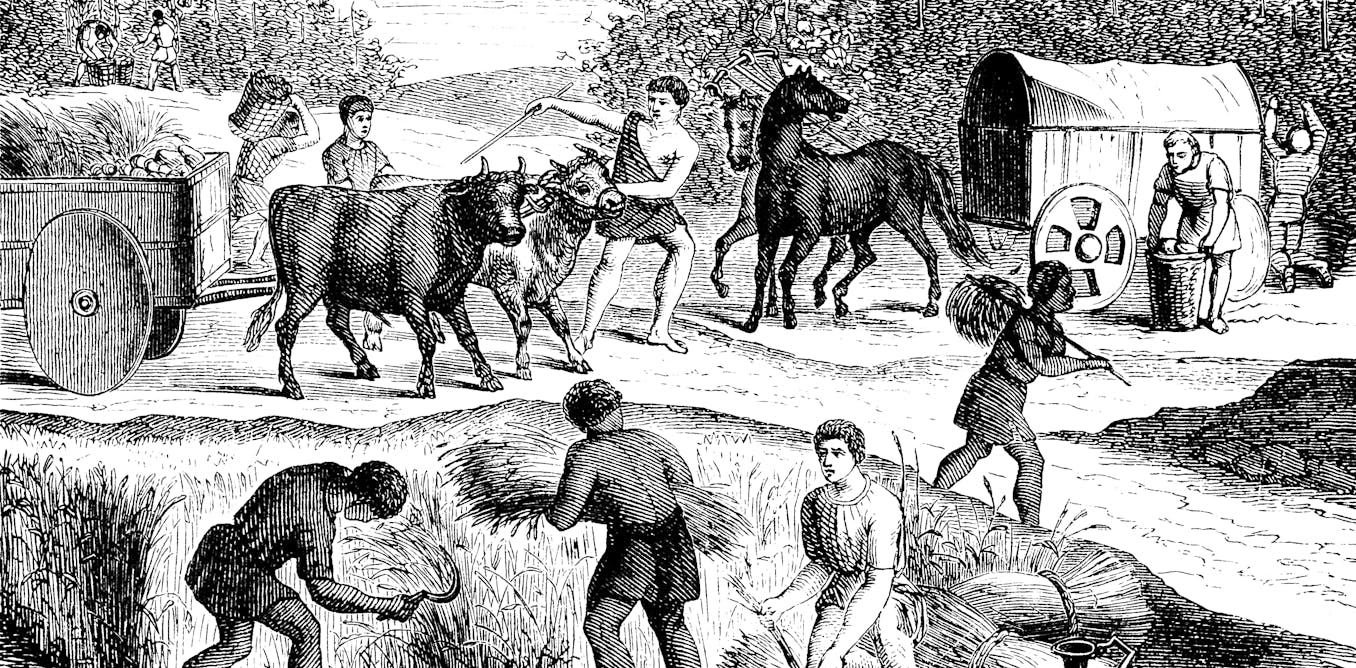
The first major wave of newly emerging infections occurred with the start of the Neolithic revolution about 12,000 years ago, when people began shifting from foraging to farming as their primary means of subsistence.
Before then, human infections tended to be mild and chronic in nature, manageable burdens of long-term parasites that people carried around from place to place. But full-time agrarian living brought the kinds of acute and virulent infections that we are familiar with today. This global shift was humanity’s first epidemiological transition.
The first emerging infections followed the rise of intensive agriculture. mikroman6/Moment via Getty Images
Farming itself was not the cause. Rather, it was the major lifestyle changes associated with this new enterprise. Agriculture supplied people with high-calorie grains, but often did so at the expense of dietary diversity, resulting in compromised immunity from nutritional deficiencies.
The human population increased dramatically, and so did the number of large and densely settled communities that could sustain the transmission of deadlier pathogens.
Our ancient ancestors domesticated animals for food and labor, and their proximity to one another created opportunities for livestock diseases to evolve into human diseases.
Finally, the social hierarchies of newly agrarian societies led to disparities in the distribution of essential resources for healthy living.
These challenges of subsistence, settlement and social organization were the root causes of humanity’s first major disease transition.
Declining Infections
For a dozen millennia, these patterns spread across the world like a plague of plagues. They persisted until the 19th and 20th centuries, when life expectancy rose with the precipitous decline of infectious diseases in high- and middle-income countries.
Remarkably, the greatest proportion of this decline occurred before the discovery of effective antibiotics and most of the vaccines we use today. Health improvements were mainly due to nonmedicinal factors such as better farming and food distribution methods, major sanitation projects and housing reforms in poor urban areas.
Urban sanitation did more than new medicines to reduce infections in the 19th century. Bettmann via Getty Images
These were significant reversals in the same ancient categories – subsistence, settlement and social organization – that led to the rise of infectious diseases in the first place. They resulted in humanity’s second epidemiological transition, a significant but only partial reversal of the changes that first began in the Neolithic period.
This second pattern was not a panacea. Despite overall health improvements, chronic noninfectious conditions such as heart disease and cancer rose to become the primary causes of human mortality.
Most low-income countries experienced a later version of this transition after World War II, but their health gains from declining infections were significantly less than those of their wealthier counterparts. At the same time, their losses to noninfectious diseases rose at comparable rates. These conflicting trends have led to a “worst-of-all-worlds” scenario with respect to the health of poor societies.
It is also worth noting that the declining infections in low-income societies have depended more on affordable antimicrobial drugs. Given the emergence of drug-resistant pathogens, these medicinal buffers are proving to be little more than short-term solutions for the health consequences of poverty.
With the ability of pathogens to move freely across borders and boundaries, these consequences can quickly become everyone’s problems.
Every corner of the globe is connected by modern travel. fotograzia/Moment via Getty Images
Converging Infections
In recent decades, humanity’s interconnections have reached the point that nearly everyone now lives within a single global disease environment. Borders and boundaries no longer constrain the spread of distant outbreaks. The COVID-19 pandemic dramatically illustrated this new reality, when the SARS-CoV-2 virus spread around the world in only a few weeks.
The COVID-19 pandemic also highlighted the ways that infectious and noninfectious diseases can interact synergistically with one another to produce even worse outcomes than the simple sum of each disease. This is starkly illustrated by the majority of COVID-19 deaths, which occurred among people with chronic heart, lung and metabolic conditions that are common to a growing proportion of older people in populations both wealthy and poor.
When combined, these challenges have set the stage for the converging disease patterns visible today. This is the third epidemiological transition: the rise of new, virulent and drug-resistant infections occurring in a rapidly aging and highly interconnected world.
Unfortunately, the present pattern entails increasing outbreaks of new and deadly infections. The root causes of these outbreaks are in areas such as commercial agricultural practices, the urbanization of human populations and the challenges of poverty in the face of economic growth.
Despite the magnitude of these determinants, they are essentially the same issues of subsistence, settlement and social organization from 12,000 years ago. Addressing these recurring issues will do more than prepare the world for future pandemics; it will help to prevent them from happening in the first place
Ron Barrett is an Associate Professor of Anthropology at Macalester College. This article is republished from The Conversation under a Creative Commons license. Read the original article.