Autopsies Have A Long and Complicated History
Posted on Categories Discover Magazine
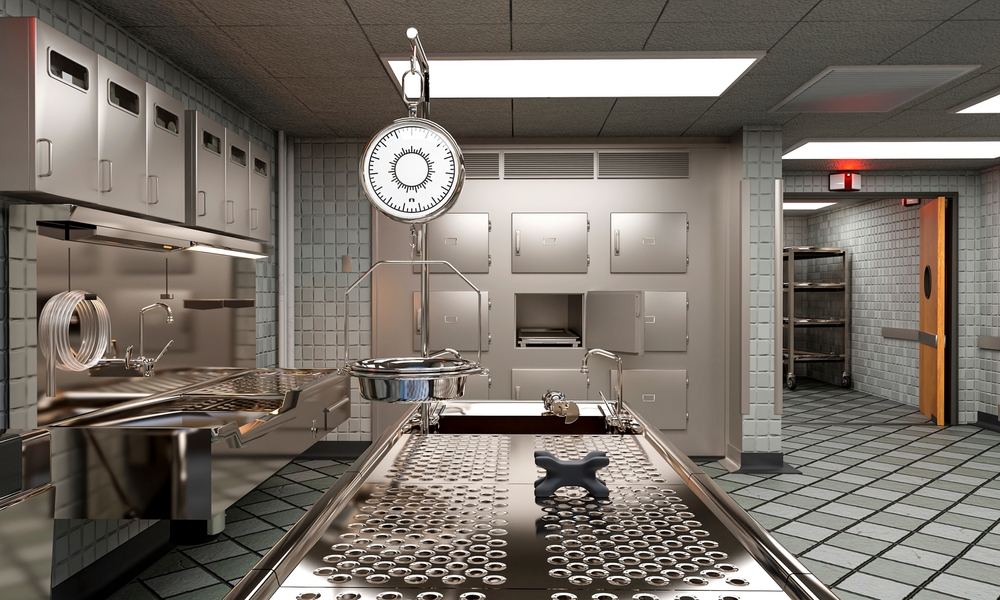
When a person dies of unknown causes, modern forensic pathologists might conduct a complete or partial autopsy. In some situations, they might use magnetic resonance imaging (MRI) or computed tomography (CT scan) to help them see deep into the body.
Although imaging technology is new for forensic pathologists, the process of conducting an autopsy to understand how a person died is an ancient practice that dates back thousands of years.
What Is an Autopsy?
An autopsy is an internal and external examination conducted on a corpse to determine the cause of death. Autopsies can help establish how a person died and whether the cause was natural or if the person died by homicide or suicide.
A forensic pathologist typically determines whether an autopsy is needed. A person who dies in hospice from cancer, for example, will likely not need an autopsy because their medical history and cause of death are well-known. This type of autopsy is known as a clinical or hospital-based autopsy. However, a person who is found dead in a forest preserve will likely undergo an autopsy because of the suspicious circumstances. This is known as a forensic autopsy.
There is also a distinction between a forensic autopsy and an anatomic dissection.
“The difference between an autopsy and an anatomic dissection is the purpose. The anatomic dissection is for research. Forensic autopsy is to determine the cause of death,” says Victor Weedn, a past president of the American Academy of Forensic Sciences.
Anatomic dissections were controversial in Europe and the U.S. for centuries because medical students often robbed fresh graves to study cadavers.
Forensic autopsies, in contrast, were only conducted when a cause of death was suspicious or unknown. This is a practice that stretches back thousands of years.
“People are really interested in who kills who, way back to the earliest of societies,” Weedn says.
Read More: Autopsies on Hold: Why We Need More Medical Examiners
Ancient Autopsies
There are records of animal autopsies dating back to ancient Egypt in 4000 B.C.E. Human autopsies date back to ancient Egypt in 3000 B.C.E. These autopsies were conducted to learn more about human anatomy and also to identify the cause of death in murder cases.
Doctors even conducted an autopsy on Roman dictator Gaius Julius Caesar after he was assassinated in the senate in 44 B.C.E., even though the cause of death was clear.
“A particular physician looked at him and said one of the 32 stab wounds was fatal,” Weedn says.
Although deaths were investigated in ancient times, there was a lack of uniformity as to how cases were approached and how evidence was handled. In the 13th century, Chinese physician Song Ci wrote The Washing Away of Wrongs, a guide meant to inform death investigators of proper procedures.
“It’s considered the first guide in forensic medicine,” Weedn says. “The Washing Away of Wrongs is really a manual for other investigators on how to investigate death. It talks about how to tell if a body in water died from suicide or homicidal drowning.”
In Europe, forensic pathology was also used to investigate death. In Bologna in 1289, for example, a judge summoned two doctors to meet him at a church to examine a deceased victim with multiple stabbings. The doctors found 11 stab wounds, which they deemed were all fatal except for one. However, the Catholic Church had a problem with the practice and was barred until the 1500s.
The Rise of Forensic Autopsy
After the Catholic Church green-lighted forensic autopsies, physicians advanced the process of investigating disease and suspicious death through autopsy. By the 1800s, pathology was considered its own discipline.
As the specialization emerged, so did the idea of having a physician for legal purposes determine the cause of death when foul play was known or suspected.
In the U.S., Maryland was the first state in 1860 to pass a law requiring that a trained physician had to be present during death inquests. Some states organized their medicolegal system so that autopsies were under the determination of a medical examiner who was a trained physician.
Other jurisdictions have maintained having an elected coroner to oversee inquests. Although a trained physician must conduct the autopsy, the coroner can choose not to order an autopsy and is responsible for certifying the results.
As medical examiners’ and coroners’ offices developed in the twentieth century, specialized physician training was not yet required.
“They didn’t have forensic pathologists as such, they were just physicians that did the work,” Weedn says.
Forensic pathology evolved to require specific training, including a pathology residency after medical school, followed by an additional fellowship in forensic pathology.
Read More: Looming Shortage of Coroners Has Historic Parallel
Future of Autopsies
Although forensic pathology will remain as long as there are suspicious deaths, advancements in technology may mean that imaging could one day replace the conventional autopsy.
In Japan, post-mortem imaging is the standard as opposed to an autopsy. The autopsy rate is only 2 percent overall. Even when a death is deemed “unusual,” a conventional autopsy is only used 11 percent of the time.
Instead, CT scans and MRIs are used to determine the cause of death. It’s a practice that more countries are considering, and conventional autopsy rates are now declining worldwide as imaging becomes more accessible and more capable.
It’s possible that in the future, the ancient practice of autopsy may one day be ancient history.
Article Sources
Our writers at Discovermagazine.com use peer-reviewed studies and high-quality sources for our articles, and our editors review for scientific accuracy and editorial standards. Review the sources used below for this article:
Emilie Lucchesi has written for some of the country’s largest newspapers, including The New York Times, Chicago Tribune and Los Angeles Times. She holds a bachelor’s degree in journalism from the University of Missouri and an MA from DePaul University. She also holds a Ph.D. in communication from the University of Illinois-Chicago with an emphasis on media framing, message construction and stigma communication. Emilie has authored three nonfiction books. Her third, A Light in the Dark: Surviving More Than Ted Bundy, releases October 3, 2023, from Chicago Review Press and is co-authored with survivor Kathy Kleiner Rubin.